OVERVIEW
Medical science keeps advancing and improving year by year – and so does the technology we use in our treatments.
One of the biggest developments in recent orthopaedics has been the introduction of robot-assisted surgery for joint replacement, which Mr Aslam has been performing at Spire Southbank Hospital since its arrival last year. Experts have described the technology as a “game-changer”, since it’s bringing new levels of precision and customisation to the knee replacement process.
What is robotic knee replacement surgery?
Traditional joint replacement is an operation for knees that have become painful and dysfunctional because the bone endings have lost their protective cartilage covering – usually due to osteoarthritis, or a previous injury. During the operation, the surgeon removes damaged material from the bones and fixes a smooth, artificial implant in their place.
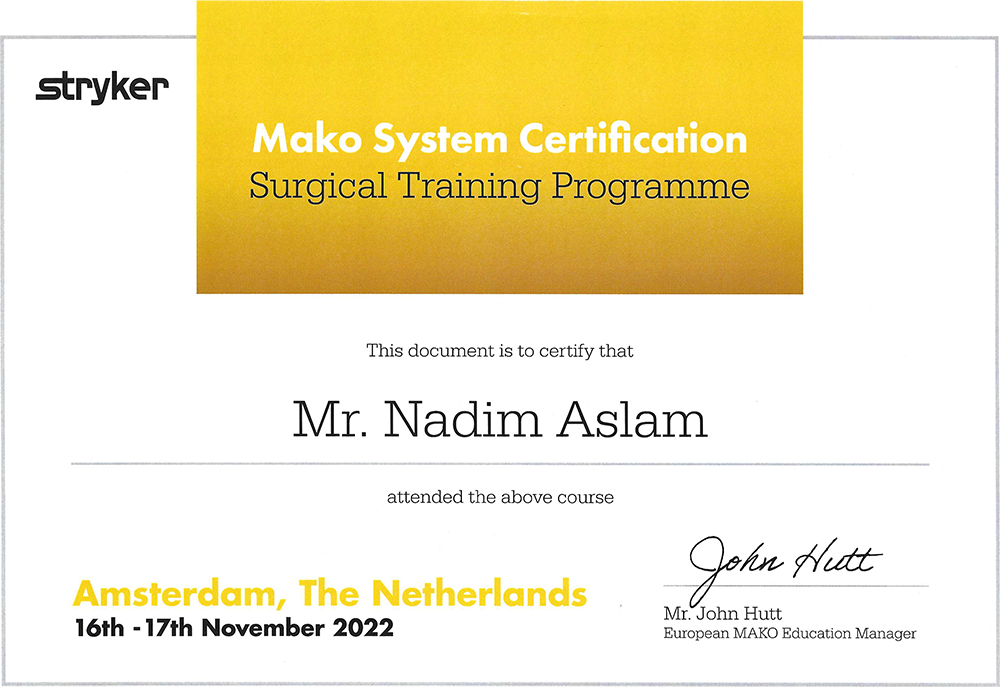
In robot-assisted joint replacement, the surgeon uses a system called the Stryker Mako to help plan and perform these operations with an exceptional degree of accuracy. The Mako brings several major benefits to the pre-operative and surgical process.
It’s bespoke – the system uses advanced 3D modelling to map the anatomy of your knee and create a detailed individual plan for your operation, well before you come into theatre. It enables us to pre-plan the exact cuts we need to make before the procedure, and tailor them precisely to your joint. See How it works, below.
It’s precise – the Mako’s robotic arm can operate within a fraction of a millimetre. Its software provides a visual path for the surgeon as he makes the planned cuts and fixes the implant, while the arm uses tactile resistance to prevent him moving outside the planned boundaries. Preserving the maximum healthy bone and tissue is important in surgery, because it helps to reduce post-operative pain and speed recovery. See What the research is saying.
It’s time-tested – although the concept sounds futuristic, Mako has actually been operating since 2006 (see our surgical timeline, below). To date more than 100,000 Mako procedures have been carried out, over 700 surgeons around the world regularly perform it, and the technology has been covered by more than 50 peer-reviewed clinical publications.
It’s natural – ultimately a surgeon’s goal in knee replacement is to create a joint that feels as natural as possible for the patient. While no kind of surgery can provide a totally guaranteed outcome, the Mako’s accuracy, predictability and tailored approach is helping us to give our patients the best chance of a ‘best-fit’ replacement.
Robot-controlled? Not exactly…
It’s worth adding that, while the technology often makes people imagine a completely autonomous machine that takes over the doctor’s job, the human surgeon stays in control of the robot through the whole operation.
The surgical component of the Mako is actually a highly calibrated arm, equipped with a specialised cutting tool: the official title is “robotic-arm assisted surgery”. Precision software guides the surgeon in making the pre-planned cuts with the arm, but the surgeon controls the arm and we can override the system at any time. In other words the Mako is more like a finely tuned assistant for the surgical team, helping to make a good operation even better.
HOW IT WORKS
- 1
The Mako process starts with a CT scan of your leg. Capturing the whole limb allows us to view the anatomical alignment of your hip, knee and ankle joints. It takes about 30mins and can be done at Southbank Hospital.
- 2
The scan takes x-ray images of your leg from multiple angles. We use the data from these images to generate a 3D virtual model of your knee. This is loaded into the Stryker Mako system to create a bespoke surgical plan for your joint, from the optimal implant size to the best angles for surgery.
- 3
When Mr Aslam has reviewed the plan and adjusted it if necessary, it’s uploaded to the Spire Southbank Hospital’s Mako robot. The robotic arm is equipped with a specialised surgical saw, which will remove the diseased portions of bone from your joint.
- 4
On the day of the operation, a trained Stryker specialist joins the surgical team to run through the procedure plan, help the team prepare the Mako in theatre, and supervise it during the operation.
- 5
Mr Aslam places reflective markers around the joint to synchronise your knee with the 3D model in the Mako system.
- 6
Mr Aslam uses the robotic arm to remove defective bone from the knee, within the boundaries set out in the plan. He stays in control of the procedure, but the Mako uses real-time feedback to guide their movements and prevent them from straying outside the boundaries (the saw actually cuts out if the surgeon tries to do this). This builds precision into the process and helps preserve the optimal amount of healthy tissue.
- 7
When the diseased bone has been removed, the Mako system ensures the implant is inserted into the joint space as planned. The surgeon carefully checks the range of movement in the knee, completes the operation and returns you to the recovery room.
- 8
When you’ve woken up, Mr Aslam will visit you to talk through the procedure and check that you have everything you need. Over the next two days, we aim to get you mobilised as soon as possible – most patients are able to take their first steps within 24 hours, and to use stairs by day two or three.
- 9
Depending on whether you’ve had a full or partial replacement, you should be ready to go home after two or three nights in hospital. We’ll see you again in two weeks to remove your stitches and dressing, and review your progress.
FREQUENTLY ASKED QUESTIONS
Stryker has worked with Surgeons to develop initiative products to be utilised in the field of orthopaedics. Mako robotic-arm assisted technology can be used for total hip, partial knee and total knee replacements. This is for patients who suffer from non-inflammatory or inflammatory degenerative joint disease. Mako technology provides me with a specific CT-based 3D model of your unique anatomy and assists me in focusing on removal of diseased bone, helping preserve healthy bone and assisting me in the positioning and precision placement of the implant more accurately.
It all begins with a CT-based scan of your joint that is used to generate a 3D virtual model of your unique anatomy. The virtual model is loaded into the Mako system software and is used to create your personalised preoperative plan. Mako allows me to make adjustments to your plan during surgery as needed. During the surgery I guide the robotic-arm within the pre-defined area so that only damaged bone is removed and the implant is aligned with pinpoint precision.
The first Mako knee and hip replacements were performed in Florida in 2006 and 2010 respectively.
The surgery is performed by me using the robotic-assisted arm, with the guidance of the CT-cased model which is programmed into the Mako system.
• Less pain than traditional hip or knee replacement surgery
• More accurate than traditional hip or knee replacement surgery
• Less blood loss
• Less muscle and tissue trauma
• Faster Recovery
• Shorter hospital stay
• Reduced hip or knee dislocation risk – okay to cross legs – okay to lie on either side
• No wedge between legs necessary
• More rapid recovery to full function
• More rapid return to driving
• Can often walk the day of surgery
• Reduced requirement for crutches
All surgery carries risks and these will be discussed at your consultation prior to surgery. Clinical studies show Mako can help to reduce certain risks including more accurate alignment of hip implants based on the surgical plan, a reduced risk of blood loss and less likelihood of hip dislocation.
If you are experiencing severe hip or knee pain due to a degenerative condition such as osteoarthritis or rheumatoid arthritis, you may be offered hip or knee replacement surgery, this will be discussed at your consultation.
Spire South Bank Hospital, 139 Bath Road, Worcester, WR5 3YB
To book a consultation contact:
Mr Nadim Aslam, Orthopaedic Robotic Surgeon, of the Worcestershire Knee & Hip Clinic
✉ [email protected]
Website: www.wkhc.co.uk
☏ 01905 362003